Rachel Bruns is a volunteer advocate for quality maternal health care in Iowa.
With the Iowa legislative session beginning January 13, it is time for a rundown of important maternal health policies that should become priorities for state lawmakers in 2025.
Since I am focusing on access to midwifery care, it is worth noting that in October 2024 the World Health Organization issued a new position paper on “Transitioning to Midwifery Models of Care.” That paper offers an international definition by describing the guiding principles of midwifery models of care and reviewing the advantages of adopting them.
According to the World Health Organization’s position paper,
More than 60% of all maternal and neonatal deaths and stillbirths could be averted by achieving universal coverage of midwife-delivered interventions by 2035, including the provision of family planning before conception,14 according to a recent modelling study (Fig. 3.1) (97). This represents 4.3 million lives of women and newborns that could be saved each year (97). Even a modest 10% increase in coverage every five years by 2035 could save 1.3 million lives annually (97).

Source: UNFPA, 2020 (98), adapted from Nove et al., 2021 (97). Reproduced with permission
Iowa has not achieved the ratio of six midwives per 1,000 births recommended by the World Health Organization. Our state has approximately 3.4 midwives per 1,000 births, according to data from the American College of Nurse-Midwives. Maternal or neonatal health initiatives that do not recognize the importance of midwifery-led care are not serious about improving outcomes in these areas.
A Bleeding Heartland post I wrote last year covered several maternal health policies, two of which Iowa enacted in 2024. It is important for folks to remember that even though the political environment may be divisive and callous, there are a few bright spots. Showing up at the capitol and speaking out about issues that matter to you can make a difference.
RECAP OF IOWA’S MATERNAL HEALTH POLICY CHANGES IN 2024
Thanks to Senate File 2251, passed during the 2024 session, Iowa will become one of the few remaining states to expand postpartum Medicaid coverage from 60 days to twelve months. That is critical to improving maternal health, as more than half of pregnancy complications in Iowa occur between 43 days to one year postpartum.
Unfortunately, the bill Governor Kim Reynolds introduced also lowered the income limit to qualify for Medicaid coverage during and after pregnancy, from 375 percent to 215 percent of the Federal Poverty Level. The nonpartisan Legislative Services Agency estimated that on average, the new income limits will mean that each month, 1,300 fewer Iowa women and 400 fewer infants will be covered by Medicaid during and after pregnancy. We will need to keep an eye on whether changing the eligibility rules affects maternal health outcomes.
Iowa’s new law on postpartum Medicaid coverage was supposed to go into effect on January 1, 2025. However, the federal Centers for Medicare & Medicaid Services didn’t approve the state’s plan until January 6, and they still need to align this with their rate adjustments. The governor’s office announced on January 7 that “the implementation date is still forthcoming.” Until then, pregnant Iowans with incomes up to 375 percent of the federal poverty level will qualify for Medicaid coverage—but postpartum coverage will extend for only 60 days, not the twelve months stipulated by the new state law.
It was a relief to learn that the final version of a bill on state boards and commissions (Senate File 2385), which passed late in the 2024 legislative session, retained the state’s Midwifery Advisory Council. That council had only just been created in 2023 with the passage of House File 265, a midwife licensing bill. The purpose of the Midwifery Advisory Council was to advise the state Nursing Board regarding Certified Professional Midwives’ licensure and related standards of practice.
Retaining this council is critical, because members of the Nursing Board do not have the capacity or knowledge on midwifery to provide appropriate oversight. As House and Senate Republicans negotiated a compromise on the governor’s proposal to eliminate dozens of state boards and commissions, House members were able to get the Senate to accept language retaining the Midwifery Advisory Council and some other boards.
With uncertainty surrounding the status of the Midwifery Advisory Council, the Nursing Board was not appropriately informing the council members of developments. Once the bill retaining the council passed, the Nursing Board issued public notice for CPM rules and a public comment opportunity took place in early June. The rules were adopted in mid-June and licensure for CPMs became available effective July 1, 2024. In less than six months, 22 Certified Professional Midwives were licensed in Iowa, with more expected to become certified and licensed in the coming year.
Aside from legislative happenings, the Iowa Department of Health and Human Services launched a new hospital directed payment program in 2024, in consultation with the Iowa Hospital Association. During a call last year with the Iowa Maternal Quality Care Collaborative, Iowa HHS Director Kelly Garcia shared that the program will bring in more than $1 billion of new revenue to Iowa hospitals, with a focus on behavioral health and maternal health quality measures. During the call it was noted that Medicaid reimbursement should no longer be a challenge for Iowa hospitals; the key remaining challenge will be staffing.
The directed payment program is currently only available to hospital-based services, and does not extend to out-of-hospital based maternity providers. With so much focus on the closure of Iowa hospital labor and delivery units in recent years, it is interesting that there has been no mainstream media coverage of this significant increase in funding for Iowa hospitals.
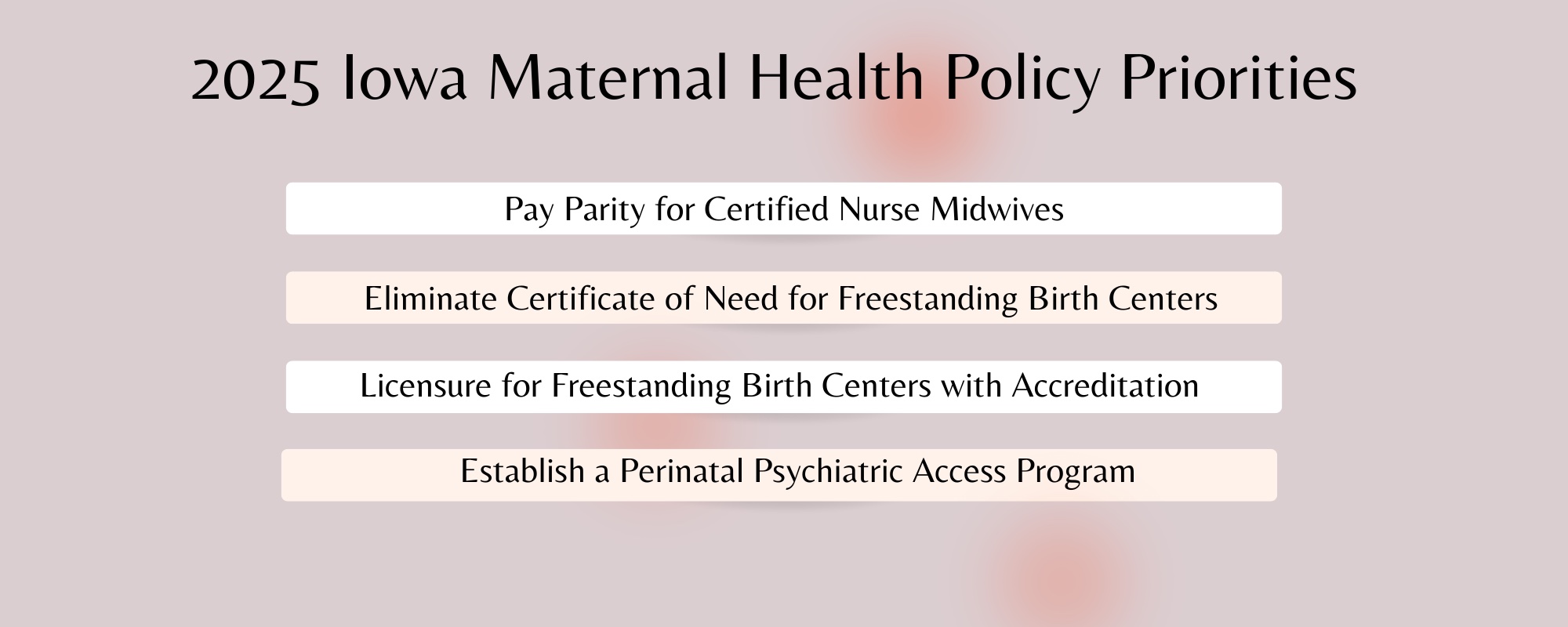
POLICIES THAT SHOULD BE PRIORITIES FOR 2025
I anticipate this year’s work will primarily focus on educating state lawmakers, as I am not aware of bills being introduced in the coming weeks on the policies described below. I highlighted some of these priorities last year, and am including two new ones for 2025.
Provide parity in Medicaid and insurance reimbursement for Certified Nurse Midwives
I have written extensively about this in the past, but here is a quick refresher. Iowa only reimburses Certified Nurse Midwives (CNMs) at 85 percent of the rate it reimburses physicians when providing the same services for gynecological and obstetrical care, such as pap smears, contraceptive family planning, prenatal/postpartum care, and vaginal deliveries.
If Iowa wants to be competitive in retaining and attracting a CNM workforce, we need to provide equal pay for equal work. Five of our six neighboring states—Minnesota, Wisconsin, Illinois, Missouri, and South Dakota—reimburse CNMs at 100 percent of the rate for physicians.
I recently learned that by not paying CNMs equitably for the same work performed by physicians, the state of Iowa likely is out of compliance with the the federal Affordable Care Act (the 2010 health care reform law). Section 2706(a) of that law prohibits discrimination based on a provider licensure in terms of (a) reimbursement of covered services which are within the provider’s state authorized scope of practice and (b) participation in any plan or insurance program.
In a related development, the American Association of Nurse Anesthesiology filed a federal complaint in September 2024 against the federal Department of Health and Human Services for not enforcing the nondiscrimination provision of the Affordable Care Act.
Eliminate the Certificate of Need for freestanding birth centers
I’ve written several times about Iowa’s Certificate of Need policy. The Iowa Senate approved a reform bill in 2023 (Senate File 506), but the Iowa House did not approve it that year or in 2024. That means advocates must start over in 2025, and State Senator Jeff Edler, who previously championed that bill, is no longer in the legislature. (He did not seek re-election last year.)
Fewer than fifteen states require a certificate of need for birth centers. Nearby states Minnesota, South Dakota, Nebraska, Kansas, Missouri, and Wisconsin do not require a certificate of need for birth centers. Iowa is also one of a handful of states that currently have no birth centers.
This 2019 report confirmed that birth centers deliver improved health outcomes at a lower cost, averaging 21 percent lower cost of birth and 15 percent lower cost for care for women and infants for the first year after birth.
In 2013, a group of Certified Nurse Midwives in northwest Iowa were denied their Certificate of Need to open a freestanding birth center due to opposition from local hospitals. In November 2024, a federal judge upheld the state’s law in a case filed by Des Moines Midwife Collective. (An appeal may be pending in that litigation.) Given that there are zero freestanding birth centers in Iowa, there is clearly a need for alternative places to give birth, especially in the 30 percent of Iowa counties classified as a maternal health desert.
Provide licensure to freestanding birth centers with accreditation
Iowa has no regulations in place for freestanding birth center licensure. Since no birth centers are now operating, that may not seem important. But it is yet another barrier for maternal health providers who want to open a birth center, in addition to the state’s lack of a birth center fee schedule. Freestanding birth centers are a critical solution to addressing maternal health care in rural Iowa, where most counties have no service providers.
The Iowa Senate’s 2023 reform bill, which would have exempted birth centers and community mental health centers from the Certificate of Need process, would have required the Department of Inspections, Appeals, and Licensing to create birth center regulations. Since the House didn’t pass the bill, Iowa continues to be without birth center regulations and licensing.
To limit unnecessary bureaucracy, Iowa should follow states like Minnesota in providing licensure for birth centers accredited by the Commission for the Accreditation of Birth Centers. This can be an alternative licensure pathway to any other requirements the state sets for non-accredited birth centers. Birth centers with such accreditation already meet high standards and adhere to industry best practices.
The federal government recognizes the importance of expanding access to birth centers; the Centers for Medicare & Medicaid Services included that concept in their new Transforming Maternal Health Model funding opportunity. However, the state of Iowa chose not to apply for that federal funding in 2024.
Establish a perinatal psychiatric access program
There is a gap between the demand for perinatal mental health services and the supply of professionals who can provide these services. While there is not one simple solution to this shortage, a Perinatal Psychiatric Access Program is an important tool to support the mental health of Iowa moms. More than half of states currently operate Perinatal Access Programs. Iowa ACES 360 is leading a broad coalition of organizations to advocate for this resource in our state.
Iowa ranks 51st out of 50 states and Washington, DC for mental health psychiatric beds and fails to meet the minimum standard for adequate treatment, according to the Treatment Advocacy Center, as the Des Moines Register has reported. Mental health conditions are the leading cause of pregnancy-related deaths in the U.S.
Perinatal psychiatric access programs are a centralized resource providing psychiatric expertise and support to front-line health care professionals (OB/GYNs, family physicians, etc.) who interact directly with pregnant and postpartum individuals. These programs provide training and education to health care providers on mental health screenings, treatment options, and referral processes. A statewide phone line offers immediate access to psychiatric consultations for guidance on patient care. In addition, resources and referrals for patients to be connected to community-based mental health resources.
Perinatal access programs are a workforce development strategy. They could boost Iowa’s maternal health workforce by providing health care providers with essential training, real-time psychiatric support, and resources. That would help them better meet the mental health needs of pregnant and postpartum individuals, effectively increasing our health care capacity. Creating such programs would enhance provider capacity, improve maternal mental health outcomes, and optimize resources use in all areas of the state.
Federal bills to watch
Here is a quick overview of federal bills to pay attention to, which would improve access to midwifery care and maternal health in Iowa.
The Midwives for MOMS Act would fund midwifery education and expand educational programs and preceptor sites. U.S. Representative Ashley Hinson (R, IA-02) will re-introduce this bipartisan bill this month as a lead sponsor. The proposal is important to Iowans because it would provide funding to educate more midwives in accredited programs. Iowa doesn’t have enough midwives, especially in rural and underserved areas.
The BABIES Act, reintroduced in 2024, would set up a demonstration of prospective payment for accredited birth centers in six states and would evaluate savings to Medicaid after a period of four years. It also includes a small amount of funding to help new birth centers get started. That would be helpful to Iowa where there are currently no birth centers. It would need to be introduced again in the new Congress.
U.S. Representative Zach Nunn (R, IA-03) is a co-sponsor of the Midwives for Service Members Act, which would establish a five-year pilot project to cover midwifery services for TRICARE beneficiaries.
Iowans interested in advocating for state legislative priorities are encouraged to join the second annual Maternal and Infant Day at the Iowa State Capitol on Tuesday, January 14. You can also contact your Iowa state legislators to let them know you care about these issues. Similarly, you can contact Iowa’s members of Congress about the federal bills, to thank them for their support or ask them to join as a co-sponsor.

2 Comments
Postpartum care
Postpartum depression is real and probably underreported. The initiative on perinatal psychiatric access program probably goes in the right direction. There is a lot of attention on mothers before and during delivery, and the next day the hospital tells them to prepare for going home and everything will be fine.
It’s a bit like marriages. Lot of money and energy spent until wedding day, and then the crowd of helpers and cheerers disappears.
Helping families have and raise children should be an increased priority to Iowa. It’s much harder to grow a family on the coasts than in the Heartland. And US population is aging.
Karl M Thu 9 Jan 8:25 AM
Thank you, Rachel Bruns
I always learn from your posts.
PrairieFan Fri 10 Jan 1:22 AM