The hits just keep on coming from the health and human services budget Iowa Republicans enacted this year.
As if big spending cuts to public health programs, child care assistance, social worker field services, the closure of four Planned Parenthood clinics, and ending on-site ombudsmen visits to nursing homes didn’t do enough to harm vulnerable people, that budget bill also called for short-changing Iowans who sign up for Medicaid.
The Reynolds administration is moving forward with the plan to end decades-long practice on covering health care for new Medicaid recipients.
Clark Kauffman reported for the Des Moines Register on August 30,
Currently, Medicaid has a retroactive-eligibility provision that provides payment for health care services that were delivered in the three months leading up to a person being formally declared eligible for Medicaid.
It’s intended to ensure that health care providers accept patients even when those individuals have yet to apply for Medicaid. It often comes into play when people are hit with an unexpected health crisis and need immediate admission to a care facility. With retroactive payment, the facilities have some assurance that Medicaid will eventually pay for the care that pre-dates the decision on eligibility.
The Iowa Department of Human Services has asked the federal Centers for Medicare and Medicaid Services for permission to eliminate the three-month time-frame and have Medicaid pay only for the care that’s delivered from the first day of the month in which the patient applies for eligibility.
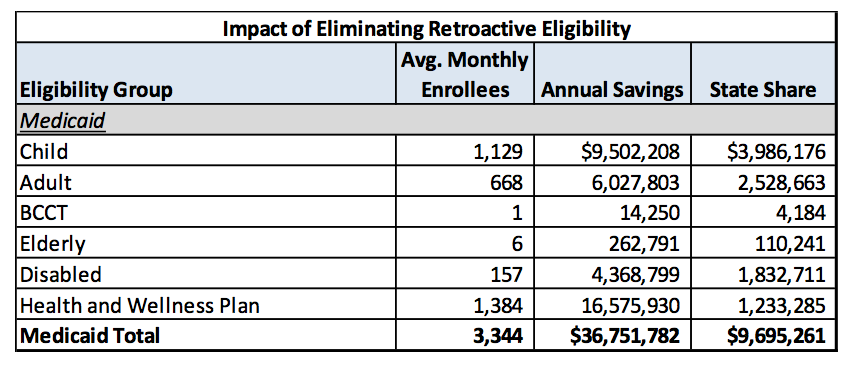
A June 2017 draft projected that the new policy would keep 3,344 Iowans off the Medicaid rolls each month, reducing annual spending by $36.8 million. The state’s share of the savings would be roughly $9.7 million per year. As this table shows, nearly $4 million of the savings would come from uncompensated care for children, $2.5 million for non-elderly adults on regular Medicaid, $1.8 million for people with disabilities, $1.2 million for those on Iowa’s version of Medicaid expansion (for those between 100 percent and 138 percent of the poverty level), and $110,000 for the elderly.
The same document put a positive spin on the change required under House File 653, the health and human services budget.
This revision will more closely align Medicaid policy with that of the commercial market, which does not allow for an individual to apply for retroactive health insurance coverage. Eliminating Medicaid retroactivity encourages individuals to obtain and maintain health insurance coverage, even when healthy. With the availability of Medicaid expansion and premium tax credits, affordable coverage options have been available in Iowa for those complying with the individual mandate, thus eliminating the need for retroactive coverage. Further, by more closely aligning Iowa Medicaid policy with policy in the commercial market, members will be better prepared if they are eventually able to transition to commercial health insurance.
The DHS received mostly-negative feedback during the public comment period in July. According to the final waiver submitted to the federal government, 23 of 27 people who weighed in opposed the idea.
Commenters opposed to the amendment noted various concerns; however, the comments generally focused on potential health and financial implications for patients and financial implications for providers. Commenters felt that the proposed change will place unnecessary financial burdens on patients/family members (19 comments), particularly those who seek services during the last few days of a month and may not apply until the following month (9 comments), those in rural locations (4 comments), or those who seek facility placement (7 comments). Commenters also focused on potential financial impacts on providers (15 comments). Eight commenters noted concerns with the potential health impacts of the amendment, indicating that future enrollees may either delay or forego needed care or be placed in inappropriate or unsafe environments.
If you’ve ever suspected state officials pay no attention to public input, this passage in the DHS application validates your concerns.
The State appreciates all comments received during the public hearings or shared with the State in writing. While all comments have been taken under consideration, no changes have been made to this application as a result of public comment. The changes proposed via this amendment are consistent with legislation passed by the Iowa legislature during the 2017 session. Specifically, House File 653 (2017) directs the State to seek a waiver from CMS to eliminate “the three-month retroactive Medicaid coverage benefit for Medicaid applicants effective October 1, 2017.”
Here’s the full request.
The Des Moines Register’s editors warned,
The people affected will not only be uninsured Iowans who never applied for Medicaid and then landed in the emergency room. They will include people who had previously secured Medicaid coverage but didn’t realize they no longer had it. […]
Unfortunately, Iowa is no longer a state that wants to ensure the poorest residents receive health care. It is now a state that seeks special federal permission to avoid paying for that care.
As of August 30, the 40 individuals or organizations who had written to the federal government to comment on Iowa’s waiver were all opposed, Kauffman reported.
The Iowa Health Care Association, which represents 800 nursing homes and assisted living centers, told CMS, “We know of no other state where CMS has taken away this benefit for this Medicaid population. We strongly encourage CMS to deny this (request) and not place the low-income elderly and disabled Iowans at risk.”
Wayne Marple, the chief financial officer for Inhance Corp., which owns two rural Iowa care facilities, told CMS, “I do not have strong enough words to describe my negative reaction” to the proposed change, pointing out that Medicaid’s $37 million in savings equates to $37 million in additional costs to be absorbed by patients or care providers.
“With the state requesting elimination of (retroactive payment), our nursing homes will no longer admit any prospective resident who is Medicaid-pending, or will become Medicaid-pending shortly after admission,” he wrote. “This will result in other providers, primarily hospitals, to incur larger amounts of charity care due to a reduced source of payment for medical services.”
My guess is that President Donald Trump’s CMS will be about as receptive to public feedback as Governor Kim Reynolds’ DHS was to the comments submitted in July.
Charged with drafting a tight budget for the current fiscal year, GOP lawmakers didn’t ask well-off Iowans or corporations to sacrifice a single extra dollar. But they called for sticking low-income people and health care providers with an extra $37 million in medical bills, in the name of saving the state $9.7 million on Medicaid. Then-Governor Terry Branstad could have item-vetoed that language, but he left it intact.
Meanwhile, the Reynolds administration has been negotiating in secret to hand over who-knows-how-much-more state and federal funds to the for-profit companies that now manage Medicaid for some 600,000 Iowans.
Your Republican Party at work.